Probing Prolactin: When High Levels Raise Red Flags
We are excited to see so many of you join our FMEP courses. Several of...
0
We are excited to see so many of you join our fall FMEP courses. Several of you have requested we continue to post more practice SAMPs, so here you go!
Just a reminder… pay attention to the questions. Here are our general tips one more time:
1. Pay attention to the questions. Look carefully at how many items you are being asked to list. If the question asks for five items, you will not get more marks if you list eight items; the examiner will look at the first five and allocate marks only for the first five answers so be careful. On a SAMP, if it is not clearly stated how many items you should list, look at the amount of points/marks being allocated for the question to get an idea of how many answers the examiner may be anticipating you write down.
2. Do not write lengthy answers. Most questions can be answered in 10 words or less!
3. Be specific when writing down investigations (hemoglobin instead of CBC; CT abdomen instead of CT).
4. Remember that trade names and generic names are both acceptable when writing down medications.
5. For more helpful tips, you can refer to CCFP’s SAMP instructions by clicking here.
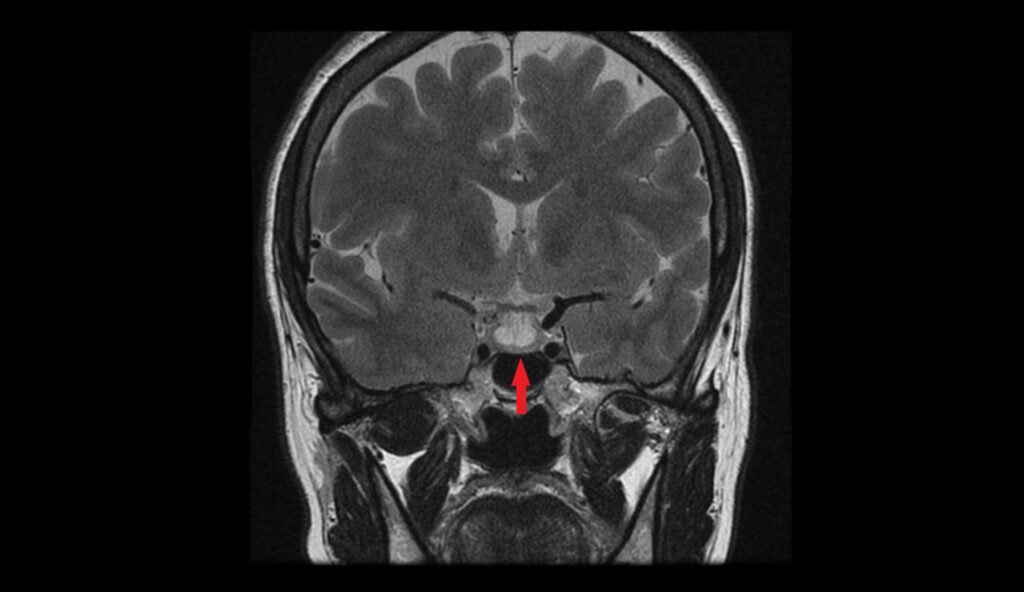
SAMP
Lai Thai is a 25 year old female who recently immigrated from Thailand. She presents to your clinic with a two-month history of difficulty closing her fist. She reports that the skin on her hands feels particularly “tight.†She also describes that her fingers turn blue when it is cold. There have been numerous red eruptions that look like spider webs on her torso and thighs. She is worried that food is getting stuck in her chest. She has smoked a pack per day for the past 10 years and uses Ventolin and Flovent which were prescribed in Thailand for a suspected diagnosis of asthma. (10 points)
1. What is the most likely underlying diagnosis? (1 point)
2. List 5 manifestations associated with the above diagnosis. (5 points) HINT: CREST syndrome.
3. True or false: This diagnosis of Systemic sclerosis is up to five times more common in males than females. (1 point)
4. What is a first-line medication used to treat this condition? (1 point)
5. She returns a few weeks later after visiting a walk-in clinic for an upper respiratory tract infection. She was prescribed prednisone 50 mg PO once daily for 5 days. What is a life-threatening complication associated with prednisone use and her underlying condition? (2 points)
References:
Denton CP, Khanna D. Systemic sclerosis. Lancet. 2017 Oct 7;390(10103):1685-1699. doi: 10.1016/S0140-6736(17)30933-9. Epub 2017 Apr 13. PMID: 28413064.
Sacino et al. (2020, July). Systemic Sclerosis. https://dermnetnz.org/topics/systemic-sclerosis.
Image by DermNet NZ, https://dermnetnz.org/
Creative Commons Attribution, https://creativecommons.org/licenses/by-nc-nd/3.0/nz/legalcode